I'm having a bad day.

I've been nominated by Nikki for the Brillante Weblog Award. I didn't prepare a 'thank you' speech, as I wasn't expecting this nomination. Oh gosh. Where do I start?
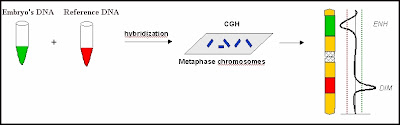
First of all, I'd like to take this opportunity to thank the driving force behind my blog - INFERTILITY. Without you kicking my ass all these years, I would not be the jealous and bitter person that I am today. Before you came into my life, I was a happy, go lucky kind of gal, skippidy-doo-dahing my way through life. And now, my life is like that of an addict - I can't wait for my next IVF fix. After all I am shooting up hormones, taking all kinds of meds, even getting some of the good stuff while they retrieve my eggs. I think I pay just about the same or even more than what an addict pays for a fix. The only difference is that I still have my house (at least for now). Thank you, Infertility, for making me a gambler. Each cycle, each egg, each embryo - I roll the dice hoping to get genetically normal embryos. But for the most part, we get mostly abnormals. I can't stop gambling. Perhaps, I should try another game like roulette. I might have better luck at spinning the big wheel and hoping it lands on my number. After all it is time that I win something back. I mean, after 3 IVFs, 1 OHSS, 3 FETs, 3 PGD/FISH, and 1 CGH - Isn't it about damn time? But until then, I just keep on bettin'.
Next, I'd like to give a special shout out to both MALE FACTOR and ROBERTSONIAN TRANSLOCATION. Male Factor, you were there from the beginning. You introduced us to the Translocation. Translocation, you are da bomb! Nobody can seem to by-pass around you. You're there whispering to us, after every PGS, to let us know just how screwed we really are. I mean, you can't mess with DNA. That's hardcore stuff there. Both of you have tried your hardest to break me. Sometimes, I even think you have a time or two or three. But that just made me even stronger and more determined.
I'd also like to thank my BIOLOGICAL CLOCK. Without you, I would not feel the pressure of each and every wasted cycle. I appreciate you for reminding me that my eggs are getting older every single day. And I may not be able to produce as many as before. So thank you for keeping count.
Next, I'd like to thank FALSE HOPE. Without you, I wouldn't be able to cry myself to sleep at night. And at my age, I need plenty of beauty sleep. Thank you for making sure I get plenty of that. You, False Hope, never disappoint me. You're always lurking in the corner, starting with my first injection; and you have stayed with me through it all.
I'd like to thank all the ASSVICE out there. Over the years, more and more of you have exploded onto the scene. When one appears two more show up as well. Sometimes, it seems that it is not possible to keep up with all of you who keep popping up. So let's break it down into the most popular categories. Let's start with Prayer. Yeah, that's a good one...Moving on. Next, there's Relax. Why don't you just shut the f-up? Next, there's Just Adopt. Um, yeah. Let's move on to Don't expect it. Oh another good one! Thank you, Assvice, for making me realize that you are all so ignorant!
I'd also like to thank all the FERTILE PEOPLE out there, who have control over when they get pregnant and how many children they want. Without your growing bellies and/or toddlers in tow, I wouldn't be reminded of the fact that your husband or significant other who may or may not be an abuser or an alcoholic or a drug user or even a deadbeat has the ability to knock you up. (Don't get your panties in a bunch. I'm just jealous.) Instead, I have to enlist a team of professionals and spend the equivalent of the FDIC insured amount, without the same guarantee of course, just to have a chance of having what you can get for free. Many of you know what it's like to just go have a drink and/or get drunk, then all of a sudden you are pregnant. Well I have kept my head on straight... no drinking, no smoking, no recreational drugs (not that I'm interested in the latter two). Perhaps I should throw caution to the wind and get drunk, do some drugs. I have enough leftover sterile needles and syringes after all. But the reality is that no matter how much alcohol I consume, it won't correct DNA. However, it may kill enough brain cells that I won't understand the concept of DNA and how hopeless our situation really is.
And last but certainly not least, I'd like to thank the UNIVERSE. I feel all the more special that you would take the time and energy, singling us out of the billions of people on earth. So an extra special thank you goes out to you, Universe, for weeding us out of the gene pool.
I know just where I'm going to put this award...right next to our 'SCREWED' trophy.

OMG, I need a drink. Hell, I need the whole damn bottle!